Preparing for Pregnancy

Why do I need to plan my pregnancy?
Planning for a pregnancy can be an exciting time. Planning is also an important step in your journey that can help promote a safe, healthy pregnancy while living with epilepsy. When you plan, you can prepare yourself for things like maintaining your seizure control and supporting your health, which will help to minimize the risk of complications during your pregnancy.
What are some of the first things I should do to plan my pregnancy?
Let’s say you are at the beginning stages of planning your pregnancy. Call your doctor and discuss when you would like to get pregnant. Each person is different, which means each person's pregnancy plan will look different from one another's. Some people want to get pregnant as soon as possible and others may want to get pregnant several years in the future. It’s recommended to start planning with your doctor as much as 12 months before you start trying to get pregnant.
One of the most important items before getting pregnant is getting your seizures as controlled as possible before getting pregnant. If you’ve tried two or more ASMs and your seizures aren’t controlled, your doctor should refer you to an epilepsy specialist.
Will I need to switch to a different anti-seizure medication before I get pregnant?
When you are pregnant, research has shown that some anti-seizure medications (ASMs) are more suitable than others. Before you try, consult with your doctor about possibly switching your ASM to one with the lowest risk profile for you and your baby that still works to control your seizures.
Ideally, any ASM changes and dose adjustments are done well before you get pregnant. Switching or adjusting your dosage can take 3-12 months, depending on the ASM you are taking. Switching or stopping medications once you’re already pregnant isn’t typically recommended. Changing medications while actively trying to conceive can unnecessarily expose your baby to multiple medications. It’s not advised to stop taking your ASM unless your doctor recommends this.
Which anti-seizure medications (ASMs) are more suitable for pregnancy?
Several ASMs have been well-studied to understand their effects during pregnancy on birth defects (also known as malformations). There are also significant findings on ASMs and their effects on other areas of fetal development (such as having lower IQ or autism spectrum disorders).
We’ve included an overview of the current research on the safety of numerous ASMs during pregnancy. Identified in green are the ‘lowest risk’ ASMs based on the data of the Maternal Outcomes and Neurodevelopmental Effects of Antiepileptic Drugs (MONEAD) study and the North American Antiepileptic and Pregnancy Registry (NAAPR).
Identified in green are antiseizure medications with the lowest risk, including lamotrigine and levetiracetam.
Identified in red is valproic acid which has been found to have the highest risk of causing fetal malformations as well as increased risk of autism with fetal exposure during the third trimester.
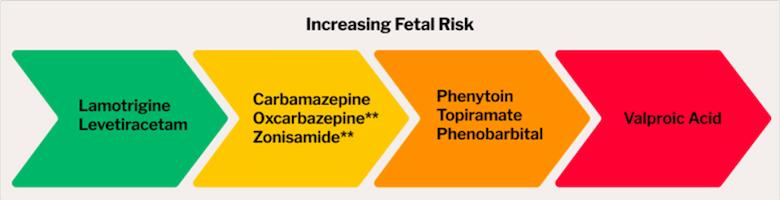
** = The neurodevelopmental risks aren’t known yet.
Other ASMs including, but not limited to, brivaracetam (Briviact), cenobamate (Xcopri), eslicarbazepine (Aptiom), ethosuximide (Zarontin), lacosamide (Vimpat), and perampanel (Fycompa) have an unknown risk.
Can epilepsy affect my fertility?
Many people worry about fertility, whether they have epilepsy or not. However, people with epilepsy are just as likely to get pregnant as people without epilepsy. According to research, there are no differences in pregnancy rates or the time it takes to conceive. There is also research that indicates fertility treatments work just as well for people with epilepsy compared to those without epilepsy.
The ASM you take for your epilepsy also shouldn’t affect your ability to get pregnant. However, some research has shown that patients with generalized epilepsy taking valproic acid are at risk of developing polycystic ovarian syndrome (PCOS). PCOS sometimes affects fertility. Consult with your epilepsy care provider if you are taking valproic acid and are concerned about PCOS.
Sometimes people have difficulty getting pregnant whether they have epilepsy or not. Let your doctors, including your epilepsy care team, know if you’ve been trying to get pregnant for six months or more. They can refer you to a fertility specialist, like an OB-GYN or reproductive endocrinologist.
Will I pass my epilepsy on to my child?
The cause of epilepsy is different for each person. It’s not likely that a parent with epilepsy will pass it on to their child. Research shows that there is only a slightly higher risk of children developing epilepsy when their parents have epilepsy (3.5-6%) than when their parents don’t have epilepsy (1-2%).
However, there are certain situations that increase the likelihood of a parent passing epilepsy to their child (e.g., when the parent has a parent or sibling with the condition). Your level of risk depends on your specific situation, so you should consult with your healthcare team if you have concerns.
Additional Information and Resources
- Pregnancy resources from the Epilepsy & Pregnancy Medical Consortium (EPMC):
- Planning your pregnancy
- Switching ASMs for pregnancy
- Choosing an obstetrician
- Heredity and epilepsy
- Epilepsy Diagnosis & Living With Epilepsy - Questions to Ask Your Doctor: Download the document for your appointment
- Epilepsy & Pregnancy Appointment Calendar- Download the calendar to keep track of appointments
- Wellness tools for epilepsy
Resources
Epilepsy Centers
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.
Epilepsy Medication
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
Epilepsy and Seizures 24/7 Helpline
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
Tools & Resources
Get information, tips, and more to help you manage your epilepsy.


