Juvenile Myoclonic Epilepsy
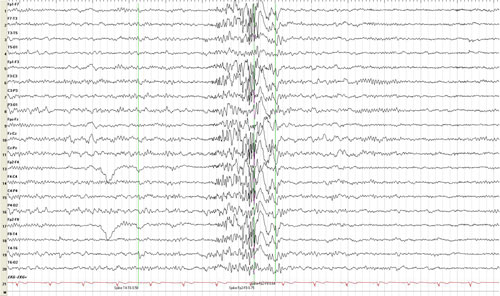
A typical EEG for JME is abnormal with 3-6 Hz generalized polyspike and wave discharge as shown here.
What is juvenile myoclonic epilepsy?
Juvenile myoclonic epilepsy (JME) is the most common generalized epilepsy syndrome. It is also called Juvenile Myoclonic Epilepsy of Janz. It usually is first seen in adolescence. Less commonly, it can develop in a child who has had childhood absence epilepsy.
Learn More:
Donate to Support Our MissionSeizure Types in JME
Myoclonic seizures are the most common seizure type and occur in everyone with JME.
- Myoclonic jerks or seizures in JME typically happen within 1 to 2 hours of waking up in the morning or after a nap.
- They are described as shock-like and irregular movements of both arms. Sometimes the movements happen only in the fingers, making the person look clumsy or prone to dropping things.
- In about 1 out of 5 people, the myoclonic jerks occur primarily on one side of the body.
- Myoclonic jerks are often triggered by lack of sleep and flashing lights.
- Not all myoclonus or muscle jerks are seizures. Many people have isolated muscle jerks that occur as they are falling asleep. These non-seizure movements are called hypnic jerks.
Myoclonic status epilepticus is rare in JME. This term describes multiple myoclonic seizures that do not readily stop. This occurs when a person first wakes up and is usually triggered by missing a lot of sleep or missing medications.
Generalized tonic-clonic seizures are seen in nearly all people with JME.
- They usually begin a few months after the myoclonic jerks start.
- These also happen in the morning when a cluster of myoclonic jerks may occur before the tonic-clonic seizure.
Absence seizures happen in less than half of people with JME.
- They are often very short (lasting less than 10 seconds) and usually don’t occur every day.
- Absence seizures with JME may not affect a person’s awareness as much as absence seizures in people with childhood or juvenile absence epilepsy.
- Both males and females are affected equally.
What can trigger seizures in people with JME?
One of the most interesting aspects of juvenile myoclonic epilepsy is that there are two very common factors that cause seizures: lack of sleep and stress.
- Lack of sleep and fatigue, primarily after drinking too much alcohol, are the most powerful causes of myoclonic jerks and generalized tonic-clonic seizures in JME.
- Mental and emotional stress are also common triggers, especially excitement or frustration.
- Some people with JME have seizures that are triggered by flickering light, such as strobe lights at dances, TV, video games, or light shining through trees or reflecting off ocean waves or snow. These are called photosensitive seizures.
Learn about managing seizure triggers
Find tips for managing stress
Is JME inherited?
Juvenile myoclonic epilepsy is a genetically determined syndrome. However, most people with JME do not have abnormal results on testing for specific epilepsy genes. About half (50 to 60%) of families with juvenile myoclonic epilepsy report seizures in either a direct relative or a cousin. The inheritance pattern is a complex type, although there are certain subtypes with distinct genetic patterns.
Learn More:
Find information about genetic testingHow is JME diagnosed?
- Your health care provider will first ask for information about what happens when you have a seizure to determine the types you have. They will also take a history of your health and your family’s health and do a physical and neurological examination.
- The EEG (electroencephalogram) is the most important test in making a diagnosis of juvenile myoclonic epilepsy.
- An EEG in untreated individuals is typically abnormal with a specific EEG pattern, known as a 3-6 Hz generalized polyspike and wave discharge. An example of this condition is shown in the figure at the top of this page.
- About a third of people with JME may show an abnormal EEG in response to flickering lights (called a photoparoxysmal response).
- MRI (magnetic resonance imaging) scans are typically normal and are not indicated (medically needed) in most cases.
How is JME treated?
- The treatment of juvenile myoclonic epilepsy starts with educating people about lifestyle and avoidance of seziure triggers.
- Avoiding sleep deprivation is essential. People with JME should make sure they get adequate rest and have appropriate outlets for emotions and stress to lessen the potential for seizures.
- It is highly advised that people avoid drinking alcohol.
- Valproic acid is the most effective seizure medication to treat juvenile myoclonic epilepsy. However, it is not the appropriate first choice to treat women of childbearing years.
- Lamotrigine is widely used for juvenile myoclonic epilepsy. Infrequently, it may lead to worsening of the myoclonic jerks even though it may help the generalized convulsions and absence seizures.
- Levetiracetam is another possible drug choice. It has been approved for treating myoclonic seizures in juvenile myoclonic epilepsy. However, it has not been well studied for all the seizure types that may be seen.
- Other possible options include topiramate, zonisamide, or clonazepam. Clonazepam given in small doses could be effective for myoclonic jerk.
- Medications that should be avoided include vigabatrin, tiagabine, gabapentin, pregabalin, phenytoin, oxcarbazepine, and carbamazepine, as these can worsen seizures, especially myoclonic jerks and absences in JME. Occasionally, carbamazepine and phenytoin may be useful for generalized convulsions.
- If seizures are not controlled, seek specialized care to determine if seizures are properly diagnosed and to explore all treatment options.
What is the outlook for people with JME?
- Seizures in most people with JME tend to improve after the fourth decade of life.
- Seizures are generally well controlled with medications in up to 90% of people.
- People who have multiple seizure types may require more medications to control them.
- It is likely that lifelong treatment with a seizure drug will be necessary, even in people with well-controlled JME. Withdrawal could result in a relapse of seizures, even in people who have been seizure free for many years with appropriate drugs.
- In some people with mild forms of the condition, the dose of seizure medication may be reduced slowly over months, particularly in older individuals. If myoclonic seizures come back or persist, medications need to be restarted.
Resources
- International League Against Epilepsy (ILAE) on juvenile myoclonic epilepsy
- National Organization for Rare Disorders (NORD) on juvenile myoclonic epilepsy
Learn More:
Contact Our HelplineResources
Epilepsy Centers
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.
Epilepsy Medication
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
Epilepsy and Seizures 24/7 Helpline
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
Tools & Resources
Get information, tips, and more to help you manage your epilepsy.



